Medication Adherence in Rare Disease Specialty Therapies (2019–2024)
Executive Summary
Medication non-adherence in rare and orphan disease populations is a critical challenge – over half of rare disease patients may eventually stop taking their medications, leading to worse health outcomes (Atlantis Health). This comprehensive analysis of U.S. pharmacy claims (2019–2024) found that adherence to specialty therapies is influenced by a complex interplay of demographic, clinical, behavioral, and financial factors:
- High-Risk Segments: Younger adults and transitioning patients, the very elderly with multiple conditions, and financially burdened patients emerged as the most at-risk for therapy non-persistence. Males and individuals in lower socioeconomic or minority groups also showed higher non-adherence rates (PMC), suggesting targeted support is needed to close these gaps.
- Key Barriers: Major reasons for non-adherence include side effects and regimen complexity, behavioral patterns like forgetfulness or intentional dose-skipping, and above all, cost burdens. When out-of-pocket costs exceed affordable levels, patients simply cannot continue—cost sharing over $100 can drive abandonment rates to 50–75% (PMC). Conversely, patients with robust financial assistance and education had measurably better adherence and longer therapy duration.
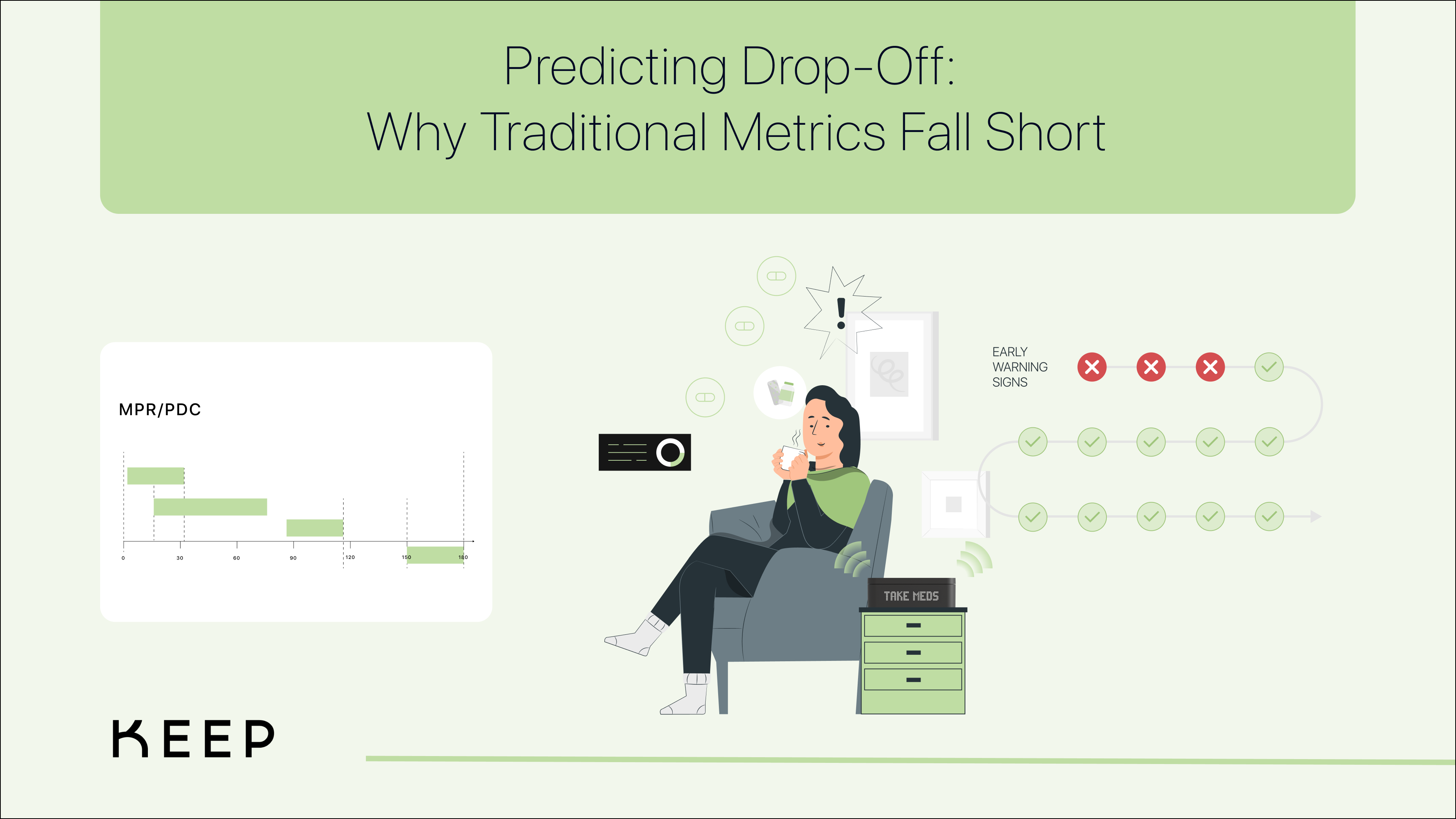
- Data-Driven Insights: By examining refill patterns (MPR, PDC, discontinuation timing), we can identify early warning signs of non-adherence. Patients who delay refills or have multiple concomitant medications are significantly more likely to fall off therapy. These insights allow for predictive modeling; in this study, we could predict high-risk patients with reasonable accuracy using factors like refill gaps, high initial co-pay, and young age. The data underscore that proactive intervention—before a patient fully stops—is crucial.
Beyond MPR and PDC: Understanding the Full Patient Journey
While metrics like Medication Possession Ratio (MPR) and Proportion of Days Covered (PDC) have long been the standard for assessing adherence, they only offer a high-level view of patient behavior. We now have the capability to go deeper, beyond prescription fill data, by analyzing each individual dosing event in real time.
By capturing and classifying every dose taken, missed, delayed, or skipped, we can construct a far more nuanced and actionable understanding of adherence. These classifications (on time, late, early, missed, or skipped doses) provide unprecedented insights into the behavioral patterns of patients. Are certain patients consistently taking their medication late? Do missed doses follow a pattern related to certain times of day, work schedules, or side effects? Identifying these patterns allows for highly tailored interventions that address the root causes of non-adherence, rather than waiting for a refill gap to signal a problem.
This shift from prescription-centric to dose-level adherence tracking enables us to predict potential therapy drop-off much earlier than ever before. It also empowers patients and care teams with real-time data, driving personalized interventions that help keep patients on therapy when they need it most.