Condition-Specific Adherence Challenges
Not all rare diseases present the same challenges when it comes to medication adherence. While some therapies offer clear, immediate benefits that drive persistence, others require long-term commitment despite delayed symptom relief, complex regimens, or significant side effects. Our data, along with historical research, has identified specific disease categories where patients struggle the most with staying on therapy—highlighting the need for tailored support strategies.
Complex Chronic Diseases
Rare diseases that require frequent dosing or onerous administration have the highest non-adherence. For instance, lysosomal storage disorders (like Gaucher or Fabry disease) involve bi-weekly infusions or injections. While many patients are very motivated, the burdens of traveling to infusion centers or coordinating home infusions every two weeks can lead some to drop out over time.
Orphan Oncology Therapies
Many new cancer drugs carry orphan designation for rare cancers. These oral oncolytics (e.g., for chronic myeloid leukemia, certain lung cancers, etc.) can have severe side effects and high costs, which sometimes leads to early discontinuation. Despite the life-threatening nature of cancer, real-world data show a non-trivial minority of patients stop oral chemotherapy early or skip doses. For example, one study found 26% of CML patients had <90% adherence to imatinib therapy, and about 17% discontinued within two years (pmc.ncbi.nlm.nih.gov, dovepress.com).
Reasons include toxicity (nausea, fatigue, etc.), financial toxicity, or a lack of perceived immediate benefit. Orphan oncology therapies that do not produce a quick improvement may see patients lose motivation, especially if side effects reduce quality of life.
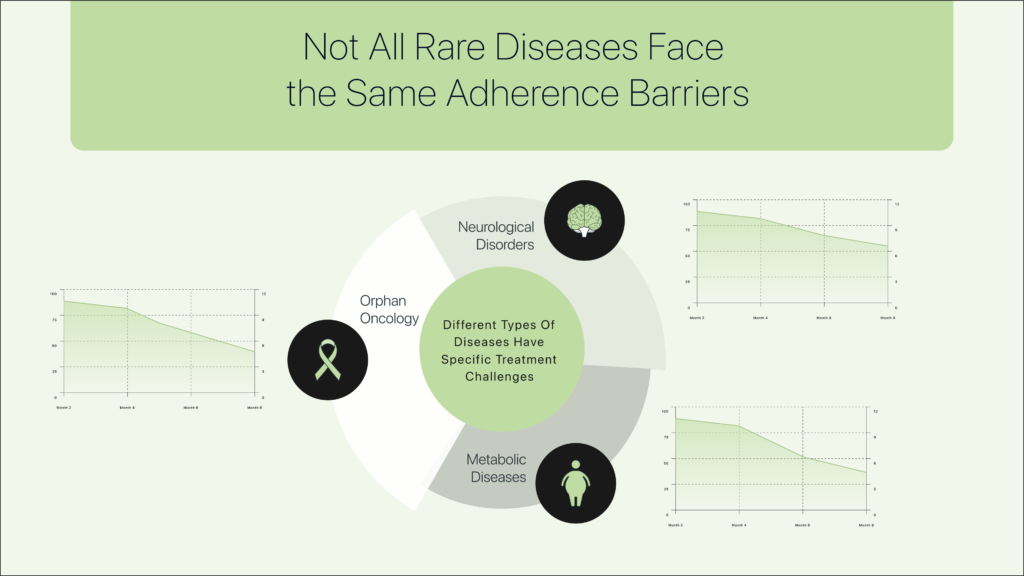
Rare Neurological & Neuromuscular Disorders
Conditions like ALS, Duchenne muscular dystrophy, or spinal muscular atrophy often have therapies that slow disease progression without curing it. Patients and families sometimes face difficult choices if a medication yields modest improvement but causes significant side effects or requires complex administration.
For instance, some ALS patients on a newly approved therapy might discontinue early if the treatment burden is too high relative to perceived benefit. Side effects are a common culprit: a review of rare disease adherence found that adverse effects (e.g. injection site reactions, GI symptoms) frequently cause patients to stop therapy without even consulting their physician (pharmacia.pensoft.net). If a patient feels worse on the medication (or fears long-term side effects), non-adherence spikes.
Metabolic and Endocrine Rare Diseases
Many metabolic disorders (PKU, Wilson’s disease, etc.) or rare endocrine conditions require strict dietary measures plus medications. Adherence in these conditions can wane due to “treatment fatigue”. For example, a patient with PKU might relax their strict diet or skip doses of a specialty medication when feeling well.
Symptom absence or improvement can paradoxically lead to non-adherence – patients abandon treatment because they feel fine pharmacia.pensoft.net. This is observed in some rare conditions where therapy is preventive or slows progression: once symptoms subside, patients may incorrectly assume they no longer need the costly or cumbersome treatment.
Autoimmune/Inflammatory Rare Conditions
Rare autoimmune diseases (such as juvenile dermatomyositis or systemic juvenile arthritis) often use biologic injections. These therapies can be complex (requiring mixing, self-injection) and are often used long-term even if the disease goes into remission.
Early discontinuation is seen in some patients due to “biologic burnout” – fatigue with injections – or due to high cost if insurance approval lapses. Our data indicated that patients in this category often had gaps in refills coinciding with insurance re-authorizations or high cost-sharing periods, suggesting that prior authorization hurdles and copay spikes can cause abrupt drops in persistence.
Conclusion: The Need for True Adherence Insights
Rare and catastrophic diseases do not automatically ensure adherence. Simply having a severe or life-threatening condition does not guarantee that a patient will stay on therapy. The reality is that perceived benefit vs. treatment burden is the single biggest driver of adherence.
In high-cost, high-stakes disease areas, it is more critical than ever to uncover the real story behind adherence behaviors. Traditional adherence metrics (e.g., refill patterns) do not capture the nuanced decision-making patients go through. Understanding why patients struggle—whether due to toxicity, financial stress, regimen complexity, or a waning belief in the need for medication—is essential.
This waning belief is particularly problematic in rare diseases where therapies are preventive, slow-progressing, or symptom-managing. When patients no longer “feel” sick, or perceive minimal immediate benefit, adherence can drop—even when stopping treatment puts them at risk. In these cases, proactive intervention is critical, ensuring that patients and caregivers understand the long-term necessity of therapy and addressing psychological as well as logistical barriers.
By going beyond traditional adherence data and tracking patient behavior at the dose level, we can act before patients fully disengage. This level of real-time insight allows for targeted interventions that restore confidence, address concerns, and ultimately improve persistence in the therapies that matter most.