High-Risk Patient Segment Profiles: Understanding Adherence Challenges in Rare Disease
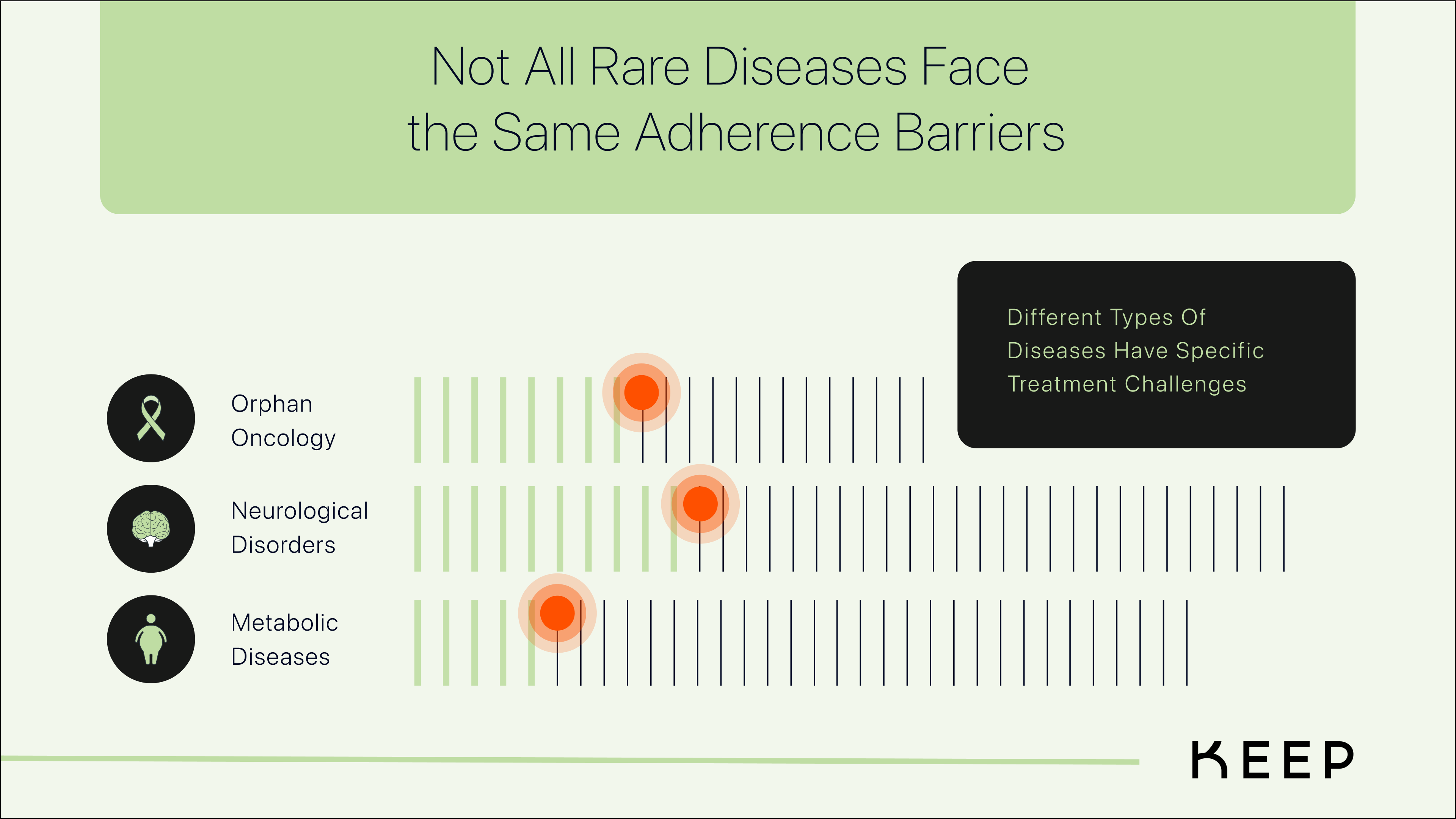
Medication adherence is never a one-size-fits-all equation. While many patients with rare diseases are highly motivated to stay on therapy, others face unique challenges that put them at greater risk of treatment discontinuation. Understanding who is most at risk and why is the first step in designing better support systems that improve long-term persistence.
By examining behavioral and claims data, several high-risk patient segments emerge—each with distinct barriers to adherence. These include young adults transitioning to self-care, elderly patients managing multiple medications, those burdened by high costs, patients navigating complex dosing schedules, and individuals lacking adequate education or support. The key to improving adherence lies in recognizing the nuances of each group’s experience and identifying the points where intervention can make the greatest impact.
Young Adults Transitioning to Self-Care: Balancing Independence and Support
For young adults managing lifelong rare diseases, the shift from parental oversight to self-management can be a difficult transition. Many of these patients have spent their childhood with caregivers structuring their medication routines, ensuring doses are taken, prescriptions are refilled, and appointments are kept. But when they reach adulthood and move out—whether for college, a new job, or simply greater independence—adherence often takes a backseat.
For some, this shift is a natural part of establishing autonomy. With new responsibilities and changing priorities, adherence can feel less urgent, especially when the consequences of missed doses aren’t immediately apparent. It’s easy to think, “I feel fine—do I really need to take this today?” Unfortunately, this mindset can lead to delayed refills, skipped doses, and, over time, full discontinuation.
The challenge here is finding the right balance between independence and structured support. Patients in this phase benefit from having a “tether” to caregivers or healthcare teams—something that provides guidance when needed, without feeling restrictive. For example, gentle check-ins or digital reminders can help them stay on track, while giving them the autonomy to manage their condition in a way that fits their evolving lifestyle.
Older Adults and the Importance of a Support Network
For older patients managing rare diseases, adherence challenges often stem from the complexity of multiple medications, cognitive or physical barriers, and a lack of structured support. Many elderly patients take ten or more medications daily, making it difficult to integrate a new specialty therapy into their regimen.
Medication storage also plays a crucial role in adherence. Out of sight often means out of mind. If a patient stores their medication in a hard-to-reach cabinet or a drawer they rarely open, doses are more likely to be forgotten. Keeping medications visible and accessible—such as near a coffee maker for morning doses—can serve as an organic reminder and improve adherence.
Beyond storage, having a circle of care attached to a patient’s dosing routine can provide additional structure. This might mean a caregiver who helps track doses, a pharmacist synchronizing refills, or even a digital tool that ensures medications are taken correctly. As aging patients navigate increasing health complexities, adherence must become a team effort, not just an individual responsibility.
Complex Dosing Schedules: The Challenge of Staying on Track
Not all rare disease therapies are simple once-a-day pills. Many involve multiple daily doses, self-injections, or alternating schedules that require careful adherence to remain effective. Over time, this complexity can lead to what’s known as “dose fatigue”—where the burden of maintaining a rigorous schedule begins to wear down a patient’s motivation.
One critical yet often overlooked issue is respecting prescribed off-days. Some therapies require breaks—perhaps injections every three days, or cycles where medication is taken for two weeks and then paused. When patients extend these off-days beyond what’s prescribed, it can disrupt treatment efficacy. A missed restart can cascade into multiple missed doses, gradually pulling the patient away from their routine altogether.
Ensuring that patients receive appropriate nudges when a cycle is about to begin again can help them maintain adherence. These reminders must be specific to the patient’s regimen—not just generic alerts but tailored notifications that prompt the correct action at the right time.
The Role of Education and Support in Adherence
For some patients, adherence is less about motivation or access and more about understanding. Many individuals—especially those who are newly diagnosed—don’t fully grasp the importance of long-term therapy. Some may believe that once symptoms improve, they no longer need their medication. Others may not realize how missing doses could impact their condition until it’s too late.
Education is a powerful adherence tool. Patients who receive clear, ongoing communication about their therapy—why it’s necessary, what to expect, and how to integrate it into their routine—are more likely to stay engaged. This education should be accessible, simple, and reinforced over time rather than provided all at once at the start of treatment.
Additionally, social support networks can play a vital role in adherence. Whether through patient advocacy groups, peer mentors, or case managers, patients who feel connected to a support system are more likely to remain committed to their treatment. No patient should feel like they are managing their condition alone.
Final Thoughts: Personalizing Adherence Support
By looking beyond generic adherence strategies and focusing on the human experience behind medication behaviors, we can build a framework that supports persistence—helping patients stay on therapy and achieve better long-term outcomes.